Reposted with permission from ©AANS, 2014
J Neurosurg Pediatrics (Suppl) 14:72–76, 2014
AANS, 2014
(Original text of the guideline was edited to reflect the update. Please click here for the original publication.)
Pediatric hydrocephalus: systematic literature review and evidence-based guidelines
Part 9: Effect of ventricular catheter entry point and position
UPDATE
Joanna Kemp, MD,1 Ann Marie Flannery, MD,1 Mandeep S. Tamber, MD, PhD,2 Ann-Christine Duhaime, MD3
1Department of Neurological Surgery, Saint Louis University, St. Louis, Missouri; 2Department of Pediatric Neurological Surgery, Children’s Hospital of Pittsburgh, University of Pittsburgh, Pittsburgh, Pennsylvania; and 3Department of Pediatric Neurosurgery, Massachusetts General Hospital, Boston, Massachusetts
Object. The objective of this guideline was to answer the following question: Do the entry point and position of the ventricular catheter have an effect on shunt function and survival?
Methods. Both the US National Library of Medicine/MEDLINE database and the Cochrane Database of Systematic Reviews were queried using MeSH headings and key words specifically chosen to identify published articles detailing the use of CSF shunts for the treatment of pediatric hydrocephalus. Articles meeting specific criteria that had been delineated a priori were then examined, and data were abstracted and compiled in evidentiary tables.
Results. The search yielded 184 abstracts, which were screened for potential relevance to the clinical question of the effect of ventricular catheter entry site on shunt survival. An initial review of the abstracts identified 14 papers that met the inclusion criteria, and these were recalled for full-text review. After review of these articles, only 4 were noted to be relevant for an analysis of the impact of entry point on shunt survival; an additional paper was retrieved during the review of full-text articles and was included as evidence to support the recommendation. The evidence included 1 Class II paper and 4 Class III papers. An evidentiary table was created including the relevant articles.
Conclusion. Recommendation: There is insufficient evidence to recommend the occipital versus frontal point of entry for the ventricular catheter; therefore, both entry points are options for the treatment of pediatric hydrocephalus. Strength of Recommendation: Level III, unclear degree of clinical certainty. (http://thejns.org/doi/abs/10.3171/2014.7.PEDS14329)
Key Words: practice guidelines, cerebrospinal fluid shunts, hydrocephalus, ventricular catheter, ventricular catheter placement, ventricular catheter position
Abbreviations used in this paper: AANS = American Association of Neurological Surgeons; CNS = Congress of Neurological Surgeons.
Shunt malfunction remains a significant source of morbidity in patients with shunted hydrocephalus. One variable affecting the risk of proximal shunt failure includes the entry point and position of the ventricular catheter. Entry from the skull is situated to access the ventricle without penetrating eloquent cortex. Although the optimal target is unclear, it has been suggested that positioning the tip of the ventricular catheter away from the wall of the ventricle and choroid plexus would improve shunt survival.
In general, entry points most often employed for this purpose have been frontal or occipital-parietal. The ventricular catheter most often terminates in the frontal horn, away from the choroid plexus, although a target in the atrium or occipital horn is used occasionally by some surgeons. Most ventricular catheters continue to be placed without use of a technical adjuvant to aid positioning.
Methods
Fourteen articles were identified using search criteria potentially related to this topic. Please see below for the specific search terms and strategies used in our search of the US National Library of Medicine database and the Cochrane Database of Systematic Reviews.
Search Terms
PubMed/MEDLINE
- (“Cerebrospinal Fluid Shunts”[MeSH]) AND “Hydrocephalus”[MeSH:noexp]
- Limit 1 to Child (0–18 years)
- 2 and ((ventricular AND (catheter OR shunt)) AND (placement OR position*))
- Limit to English and Humans Number = 183
Cochrane Database
- MeSH descriptor Child
- MeSH descriptor Infant
- 1 or 2 and (MeSH descriptor Cerebrospinal Fluid Shunts)
- 3 and (MeSH descriptor Hydrocephalus)
- 4 and (ventricular NEAR/2 (catheter OR shunt))
Search Strategies
The search yielded 184 abstracts, which were screened for potential relevance to the clinical question of the effect of ventricular catheter entry site on outcome. An initial review of 183 abstracts led to the identification of 14 papers that met the inclusion criteria, and these were recalled for a full-text review. After review of these articles, only 4 papers were deemed relevant for an analysis of the effect of entry point and position of the ventricular catheter in pediatric patients; an additional paper was retrieved during the review of full-text articles. Thus a total of 5 articles were included as evidence to support the recommendation (Fig. 1).
For each article included in the evidentiary table (Table 1), the study type, summary findings, and major conclusions were recorded, and a preliminary data class was assigned. The Pediatric Hydrocephalus Systematic Review and Evidence-Based Guidelines Task Force met to discuss the ranking of the evidence and the classification of data. Recommendations were then made based on the strength of the data in the evidentiary table. In these discussions, if a disagreement was encountered among members, a blinded vote was held and a consensus or majority opinion was reached.
Authors performed an updated literature search (in PubMed and Cochrane Central) for this guideline chapter through a medical librarian at the Congress of Neurological Surgeons Guidelines office using the below-mentioned existing search terms to update the original search through November 30, 2019. An additional 6 studies out of the 76 yielded by the 2020 update were recalled for full text review. Three of those studies met inclusion criteria from the original guideline and were included (Fig. 2)
Results
An initial review of the available literature indicated that an occipital entry for the ventricular catheter may be associated with longer shunt survival. In a study by Tuli and colleagues1 published in 1999, the authors performed a post hoc analysis of data collected during a randomized controlled trial of initial shunts placed in children between birth and age 18 years. The authors reviewed the characteristics of catheter tips and defined their locations as being the frontal horn, occipital horn, body of the lateral ventricle, third ventricle, embedded in brain, or unknown. The authors found that the occipital location was associated with a higher survival rate (HR 0.45; 95% CI 0.28–0.74; p = 0.001) than the frontal location (HR 0.60; 95% CI 0.39–0.91; p = 0.02).1
In a study by Bierbrauer et al2, a prospective analysis of catheter position revealed that 70% of shunts placed posteriorly did not require revision, compared with 59% of shunts placed in the frontal location. A life-table analysis between these groups showed a statistically significant difference in shunt survival that favored the occipital location. However, the strength of the study was diminished by the relatively weak randomization (by odd or even month of shunt placement) used to assign the treatment groups. A large retrospective study of 1719 patients conducted by Sainte-Rose et al3 demonstrated similar findings: a lower risk of proximal occlusion in catheters whose tips were in the atrium of the ventricle than in catheters whose tips were in the frontal horn (p < 0.001). The difference in the rates of proximal occlusion primarily occurred during the 1st year after insertion.
The occipital entry point may be advantageous in infants due to the effects of skull and brain growth on final catheter position.2 Nakahara et al4 demonstrated that in shunts placed in infancy, there was a higher degree of ventricular catheter shortening as well as bur hole migration, with growth relative to the ventricle when a frontal location was used. This may result in suboptimal catheter placement over time, even if the initial placement is optimal.4
These results contrast with those of a retrospective review by Albright et al5 published in 1988. That study indicated that the frontal entry location was advantageous with regard to shunt longevity in a series in which most patients were younger than 1 year of age and 90% of cases represented initial shunt placements. The authors noted that shunts inserted at a frontal location were more likely to be optimally placed, leading to longer function. They also analyzed optimally placed shunts inserted at both occipital and frontal entry points, finding improved shunt survival when the devices were inserted via frontal entry, compared with shunts placed with occipital entry, with a long-term function of 70% compared with 40%, respectively. These authors’ analysis was flawed, however, by a data collection in which there were many case omissions, as described in the Methods section.
Evidence suggests that having the catheter in an optimal position, surrounded by CSF, may also improve outcomes. Positioning the catheter in this manner is believed to reduce the risk of obstruction by choroid plexus, ependyma, or glial tissues.6 In the study conducted by Tuli et al1, the environment of the ventricular catheter tip was described as surrounded by CSF, touching brain (one side of the ventricular catheter tip in apposition to the ventricular wall), or surrounded by brain (catheter tip in the ventricle, but no visible surrounding CSF). Improved shunt survival was found in patients in whom catheters were surrounded by CSF compared with those in whom shunt tips were surrounded by brain (HR 0.21, 95% CI 0.094–0.45; p = 0.0001). This variable was found to be the greatest predictor of shunt failure, regardless of the location of the catheter tip.1
2020 Update
Whitehead et al7 looked at a gradually increasing database of studies, representing a larger number of cases. Although this is a large, multicenter study, the study is class III because it is a secondary analysis of information gleaned from different studies. There was also no randomization or control for ventricular catheter entry site. The authors did find that frontal entry site had a prolonged shunt survival time when compared to other sites. Two other studies8,9 also provided similar class III, single center, retrospective data.
Excluded Articles
Multiple papers were identified but excluded due to their lack of relevance to this specific question as well as to the population studied. Farahmand et al10 analyzed the entry point of the ventricular catheter in adult patients as a risk factor for shunt failure, but in that study the follow-up period was only 6 months. That prospective study showed that in the first 6 months after insertion, shunts inserted through a right frontal entry point had lower rates of revision (11.6%; p < 0.001) than those inserted via occipital approaches: right occipital (26.5%; p = 0.003) and left occipital (46.7%; p = 0.024). While these results are worth noting, given the adult-only patient population, we did not include the data in the pediatric recommendations.10
Another study that we reviewed sought to describe the utility of endoscopic placement of the ventricular catheter, but its analysis did not include sufficient data on entry point. The authors noted in the demographic data where the entry point was located but did not separate groups for analysis. The authors did note, however, that in this patient group a greater distance between the choroid plexus and the catheter tip reduced the risk of failure.11
Finally, we reviewed a report by Albright et al. from 2010.12 While those authors did comment on entry point, their paper was a survey of pediatric neurosurgeons that sought to assess trends and was considered to contain in- sufficient quantitative evidence for inclusion in our recommendation.
The remaining studies13-19 were found to have no information relevant to the study question and were excluded. A report by Berry et al13 was a retrospective multicenter study covering a large population that did not contain discrete information about entry site. Howard et al14 presented a technical note regarding improvement of catheter positioning for occipital entry. Kast and colleagues15 discussed shunt failure, including ventricular catheter failure, without including any information about entry point. In their 2002 paper, Robinson and coworkers16 focused on the impact of valve pressure on shunt longevity without addressing variable ventricular catheter positions. Sood et al17 presented data on the use of a ventricular reservoir at the shunt site, not ventricular catheter position; and Thomale and associates19 evaluated ventricular catheter design, not position. Finally, Steinbok et al18 used only the occipital entry site in their practice.
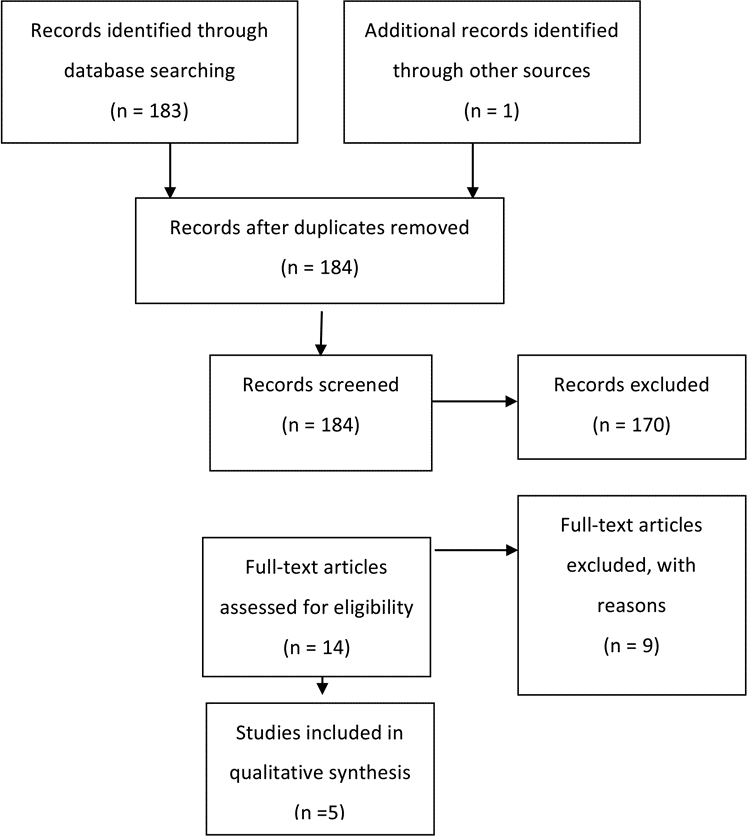
Fig. 1. Flowchart showing the process involved in identifying relevant literature.
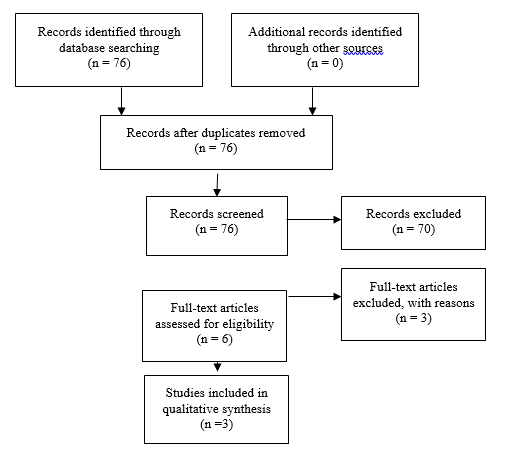
Fig. 2. Flowchart showing the process involved in identifying relevant literature for the 2020 Update. The criteria for “records excluded” and “full text articles excluded with reasons” are detailed in Part 1 of the Guidelines.
Conclusions
Recommendation: There is insufficient evidence to recommend the occipital versus frontal point of entry for the ventricular catheter; therefore, both entry points are options for the treatment of pediatric hydrocephalus. Strength of Recommendation: Level III, unclear degree of clinical certainty.
It is unclear which variable (entry point and/or catheter location) affects shunt survival. In other words, frontal versus occipital entry does not completely determine ultimate catheter position. For example, most frontally placed shunts end up in the frontal horn, but some can also end up in the body of the ventricle or the brain. Occipital placement may result in a catheter situated in the occipital horn, atrium, or frontal horn. In no study did researchers analyze patient factors such as preoperative configuration of the ventricles as a factor in the choice of entry site or shunt survival. The creation of conclusive recommendations or guidelines for the entry point or position of a ventricular catheter is impeded by the limited amount of existing evidence and, in most reports, by the lack of a multivariate analysis accounting for patient age at surgery, ventricular configuration, etiology, and other factors that might be relevant to clinical decision making. Review and evaluation of available evidence leads to the recommendation that either entry is acceptable and decisions about catheter entry site should be made based on the clinical scenario and the surgeon’s experience. The evidence would seem to support attempts to position the catheter tip so that it is surrounded by CSF and does not contact adjacent tissues. As is often the case, additional randomized controlled studies or comparative effectiveness approaches with larger data sets would provide better evidence to support a stronger recommendation. The use of technical adjuvants to achieve that goal leads to the discussion found in Part 3.
In conclusion, there is no new evidence from the 2020 Update to substantially change the original recommendations, that the frontal and occipital entry points are options for the treatment of pediatric hydrocephalus.
Acknowledgments
We acknowledge the American Association of Neurological Surgeons (AANS)/Congress of Neurological Surgeons (CNS) Joint Guidelines Committee for their review, comments, and suggestions; Laura Mitchell, Guidelines Project Manager for the CNS, for her contributions; Pamela Shaw, research librarian, for her assistance with the literature searches; Kevin Boyer for his assistance with data analysis; and Sue Ann Kawecki for her assistance with editing. We also acknowledge the following peer reviewers for their contributions to review the update to the guidelines: Jennifer Sweet, MD, Brandon Rocque, MD, Christoph Greissenauer, MD, Jeffrey Olson, MD.
Disclosure
The systematic review and evidence-based guidelines were funded exclusively by the CNS and the AANS Pediatric Section, which received no funding from outside commercial sources to sup- port the development of this document.
Conflict(s) of Interest: None. All Task Force members declared any potential conflicts of interest prior to beginning work on this evidence review.
Conflict(s) of Interest: None. All Pediatric Hydrocephalus Systematic Review and Evidence-Based Guidelines Update Task Force members declared any potential conflicts of interest prior to beginning work on this systematic review and evidence-based guidelines.
Author contributions to the study and manuscript preparation include the following. Conception and design: AANS/CNS Joint Section on Pediatrics. Acquisition of data: all authors. Analysis and interpretation of data: all authors. Drafting the article: Kemp. Criti- cally revising the article: all authors. Reviewed submitted version of manuscript: all authors. Approved the final version of the manuscript on behalf of all authors: Flannery. Administrative/technical/material support: all authors. Study supervision: Flannery.
Table 1. Effect of Ventricular Catheter Position Evidence Table
| Author |
Study Description |
Data Class, Quality and Reasons |
Results and Conclusions |
|
Bierbrau et al., 1991
|
Prospective, randomized by month, study of new shunt insertion
July 1988 to October 1990,
N=121, Follow up 2-30 months
|
Class II RCT, weak randomization, although both groups statistically similar. No assurance of blinded enrollment
Chi square analysis of data, life table analysis of shunt survival
|
Z value 1.74 for posterior versus anterior, p=<0.05.
Conclusion: longer shunt survival with posteriorly placed shunts |
|
Nakahar et al., 2009
|
Retrospective review
Review of 130 charts, excluded 102 for inadequate data.
Evaluated 28: 9 frontal, 119 parietal occipital
Mean age: 4.7 and 4.5 months
Follow up average: 78.6 and 93.9 months
Computed Tomography (CT) and plain skull radiographs measured |
Class III
No statistical analysis
|
Mean shortening of ventricular catheter in frontal group(A) was 0.83, in P/o group b it was 0.99
Burr hole displacement in a was 1.29 axial, and 1.38 lateral
In group(B) the displacement was 1.08 and 1.07
Conclusion: Shortening of ventricular catheter was more pronounced in the frontal position in the age group |
|
|
Albright, et al., 1988
|
Retrospective chart review,
180 records reviewed at 2 institutions from 1978-1981,
114 children included, CT scans available for 83 patients.
4 surgeons, plus “others”
|
Class III
Chi square analysis of variables, logistic regression, and life table analysis with time to first malfunction as “survival.”
Statistical significance less than or equal to p value of 0.05.
|
Two groups were similar in age, cause of hydrocephalus, and infection.
Also considered catheter position as independent variable (Figure 2).
Conclusion: statistically significant better long-term survival in frontal group compared to parietal per life table analysis (Wilcoxon, p=0.0008, Savage, p=0.0015 |
|
|
Tuli et al., 1999
|
Multi-center randomized trial, secondary data analysis,
344 patients randomized at 12 centers followed for 2 years, blinded review of images,
Comparability of groups commented on in prior publications
|
Class III, secondary end points, post-hoc analysis
Kaplan–Meier estimated shunt survival
Cox regression to evaluate variables.
|
Occipital entry site had the highest survival rate (HR,0.45, 95%CI,0.28-0. 74;p=0.001) versus frontal (HR,0.60;95%,CI, 039-0.91;p=0.02).
Tip position surrounded by CSF also decreased risk of failure by half (HR;0.21;95%CI0.094-0.45;p= 0.0001).
Conclusion: occipital catheters may have better long term survival, but catheter tip location may be more important |
|
Sainte-Rose et al., 1991
|
Retrospective review of 1,719 patients from 1973 to 1984, 2 institutions
|
Class III retrospective, uncontrolled chart review
|
Catheter located in the frontal horn was more likely to obstruct than catheter located in the atrium from occipital route (p<0.001).
|
|
Table 2. New evidence included in 2020 Update
| Author |
Study Description |
Data Class, Quality and Reasons |
Results and Conclusions |
|
Whitehead et al, 2017
|
This is a large, multicenter study.
|
III
|
This is a secondary analysis of information gleaned from different studies. |
|
Janson et al, 2014
|
This is a single center retrospective study. This is a largely adult study, although they did report the pediatric data separately. Nevertheless, again there is no control for site of entry or randomization. |
III
|
No new evidence is available to substantially change the prior recommendation that the frontal and occipital entry points are options |
|
|
Buster et al, 2016
|
This paper was termed a prospective and retrospective cohort study but is a single center. There is no randomization or control for a site of entry in the design of the study.
|
III
|
No new evidence is available to substantially change the prior recommendation that the frontal and occipital entry points are options |
|
|
References
- Tuli S, O'Hayon B, Drake J, Clarke M, Kestle J. Change in ventricular size and effect of ventricular catheter placement in pediatric patients with shunted hydrocephalus. Neurosurgery. 1999;45(6):1329-1333; discussion 1333-1325.
- Bierbrauer KS, Storrs BB, McLone DG, Tomita T, Dauser R. A prospective, randomized study of shunt function and infections as a function of shunt placement. Pediatric neurosurgery. 1990;16(6):287-291.
- Sainte-Rose C, Piatt JH, Renier D, et al. Mechanical complications in shunts. Pediatric neurosurgery. 1991;17(1):2-9.
- Nakahara K, Shimizu S, Utsuki S, et al. Shortening of ventricular shunt catheter associated with cranial growth: effect of the frontal and parieto-occipital access route on long-term shunt patency. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2009;25(1):91-94.
- Albright ALH, S. J.; Taylor, F. H. Function of parietal and frontal shunts in childhood hydrocephalus. Journal of neurosurgery. 1988;69(88):883-886.
- Sekhar LN, Moossy J, Guthkelch AN. Malfunctioning ventriculoperitoneal shunts. Clinical and pathological features. Journal of neurosurgery. 1982;56(3):411-416.
- Whitehead WE, Riva-Cambrin J, Kulkarni AV, et al. Ventricular catheter entry site and not catheter tip location predicts shunt survival: a secondary analysis of 3 large pediatric hydrocephalus studies. Journal of neurosurgery Pediatrics. 2017;19(2):157-167.
- Janson CG, Romanova LG, Rudser KD, Haines SJ. Improvement in clinical outcomes following optimal targeting of brain ventricular catheters with intraoperative imaging. Journal of neurosurgery. 2014;120(3):684-696.
- Buster BE, Bonney PA, Cheema AA, et al. Proximal ventricular shunt malfunctions in children: Factors associated with failure. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia. 2016;24:94-98.
- Farahmand D, Hilmarsson H, Hogfeldt M, Tisell M. Perioperative risk factors for short term shunt revisions in adult hydrocephalus patients. Journal of neurology, neurosurgery, and psychiatry. 2009;80(11):1248-1253.
- Kestle JR, Drake JM, Cochrane DD, et al. Lack of benefit of endoscopic ventriculoperitoneal shunt insertion: a multicenter randomized trial. Journal of neurosurgery. 2003;98(2):284-290.
- Albright AL. Hydrocephalus shunt practice of experienced pediatric neurosurgeons. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2010;26(7):925-929.
- Berry JG, Hall MA, Sharma V, Goumnerova L, Slonim AD, Shah SS. A multi-institutional, 5-year analysis of initial and multiple ventricular shunt revisions in children. Neurosurgery. 2008;62(2):445-453; discussion 453-444.
- Howard MA, 3rd, Srinivasan J, Bevering CG, Winn HR, Grady MS. A guide to placement of parietooccipital ventricular catheters. Technical note. Journal of neurosurgery. 1995;82(2):300-304.
- Kast J, Duong D, Nowzari F, Chadduck WM, Schiff SJ. Time-related patterns of ventricular shunt failure. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 1994;10(8):524-528.
- Robinson S, Kaufman BA, Park TS. Outcome analysis of initial neonatal shunts: does the valve make a difference? Pediatric neurosurgery. 2002;37(6):287-294.
- Sood S, Canady AI, Ham SD. Evaluation of shunt malfunction using shunt site reservoir. Pediatric neurosurgery. 2000;32(4):180-186.
- Steinbok P, Poskitt KJ, Cochrane DD, Kestle JR. Prevention of postshunting ventricular asymmetry by transseptal placement of ventricular catheters. A randomized study. Pediatric neurosurgery. 1994;21(1):59-64; discussion 65.
- Thomale UW, Hosch H, Koch A, et al. Perforation holes in ventricular catheters--is less more? Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2010;26(6):781-789.