Guidelines on the Evaluation and Treatment of Patients with Thoracolumbar Spine Trauma
11. Surgical Approaches
download pdf Neurosurgery, 2018
Sponsored by: Congress of Neurological Surgeons and the Section on Disorders of the Spine and Peripheral Nerves in collaboration with the Section on Neurotrauma and Critical Care
Endorsed by: The Congress of Neurological Surgeons (CNS) and the American Association of Neurological Surgeons (AANS)
Paul A. Anderson, MD,1 P. B. Raksin, MD,2 Paul M. Arnold, MD,3 John H. Chi, MD, MPH,4 Andrew T. Dailey, MD,5 Sanjay S. Dhall, MD,6 Kurt M. Eichholz, MD,7 James S. Harrop, MD,8 Daniel J. Hoh, MD,9 Sheeraz Qureshi, MD, MBA,10 Craig H. Rabb, MD,11 Michael G. Kaiser, MD,12 and John E. O’Toole, MD, MS13
1. Department of Orthopedics and Rehabilitation, University of Wisconsin, Madison, Wisconsin
2. Division of Neurosurgery, John H. Stroger, Jr. Hospital of Cook County and Department of Neurological Surgery, Rush University Medical Center, Chicago, Illinois
3. Department of Neurosurgery, University of Kansas School of Medicine, Kansas City, Kansas
4. Department of Neurosurgery, Harvard Medical School, Brigham and Women’s Hospital, Boston, Massachusetts
5. Department of Neurosurgery, University of Utah, Salt Lake City, Utah
6. Department of Neurological Surgery, University of California, San Francisco, San Francisco, California
7. St. Louis Minimally Invasive Spine Center, St. Louis, Missouri
8. Departments of Neurological Surgery and Orthopedic Surgery, Thomas Jefferson University, Philadelphia, Pennsylvania
9. Lillian S. Wells Department of Neurological Surgery, University of Florida, Gainesville, Florida
10. Department of Orthopaedic Surgery, Weill Cornell Medical College, New York, New York
11. Department of Neurosurgery, University of Utah, Salt Lake City, Utah
12. Department of Neurosurgery, Columbia University, New York, New York
13. Department of Neurological Surgery, Rush University Medical Center, Chicago, Illinois
Correspondence:
Paul A. Anderson, MD
Professor, Department of Orthopedics & Rehabilitation
University of Wisconsin
UWMF Centennial Bldg.
1685 Highland Ave, 6th Floor
Madison, WI 53705-2281
Email: anderson@ortho.wisc.edu
Keywords: Anterior decompression and fusion, combined anterior and posterior approach, posterior instrumentation, surgical approach, surgical treatment, thoracolumbar fractures
Abbreviations
AANS - American Association of Neurological Surgeons
CNS - Congress of Neurological Surgeons
NASS - North American Spine Society
TLIF - Transforaminal interbody decompression and fusion
ABSTRACT
Background: Modern surgical approaches include anterior decompression and fusion, posterior instrumentation with or without decompression, and combined anterior-posterior approach. However, there is variation in practice, and no consensus exists with respect to the optimal approach to surgical treatment of thoracolumbar fractures.
Objective: To determine whether there are differences in clinical and radiologic outcomes or risk of complications among anterior, posterior, and combined anterior-posterior approaches for the surgical treatment of thoracolumbar fractures.
Methods: The authors performed a thorough literature search to identify cohort or randomized clinical trials that compared outcomes of patients treated by anterior, posterior, or combined anterior-posterior approach. The outcomes of interest included clinical and neurologic outcome, radiologic outcomes, and incidence of complications. The quality of each study was evaluated, and the authors developed evidence-based guidelines.
Results: A total of 11 studies met inclusion criteria, including 4 level II randomized clinical trials, 6 level III retrospective cohort studies, and 1 level III prospective cohort study. There were no differences in clinical and radiographic outcomes, when comparing anterior only to posterior only approaches, while there were conflicting results regarding complication risks. The combined anterior-posterior approach compared to the posterior approach also showed no difference in clinical outcomes, but conflicting results with respect to radiologic results and complication risks were reported.
Conclusion: Anterior, posterior, or combined anterior-posterior approaches are all reasonable treatment options for the surgical management of patients with thoracolumbar fractures, as there was no definitive difference in outcomes or complications risk when comparing these surgical approaches.
RECOMMENDATIONS
|
Question
|
|
Does the choice of surgical approach (anterior, posterior, or combined anterior-posterior) improve clinical outcomes in patients with thoracic and lumbar fractures?
|
|
Recommendations
|
|
In the surgical treatment of patients with thoracolumbar burst fractures, physicians may use an anterior, posterior, or a combined approach as the selection of approach does not appear to impact clinical or neurological outcomes.
|
|
Strength of Recommendation: Grade B
|
|
With regard to radiologic outcomes in the surgical treatment of patients with thoracolumbar fractures, physicians may use an anterior, posterior, or combined approach because there is conflicting evidence in the comparison among approaches.
|
|
Strength of Recommendation: Grade Insufficient
|
|
With regard to complications in the surgical treatment of patients with thoracolumbar fractures, physicians may use an anterior, posterior, or combined approach because there is conflicting evidence in the comparison among approaches.
|
|
Strength of Recommendation: Grade Insufficient
|
INTRODUCTION
Goals and Rationale
This clinical guideline was created to improve patient care by outlining the appropriate information gathering and decision-making processes involved in the evaluation and treatment of patients with thoracolumbar spine trauma. The surgical management of these patients often takes place under a variety of circumstances and by various clinicians. This guideline has been created as an educational tool to guide qualified physicians through a series of diagnostic and treatment decisions to improve the quality and efficacy of care.
The surgical management of thoracolumbar fractures is highly variable. The objectives of surgical treatment of thoracolumbar fractures are to decompress neural elements when required, realign the spine, reduce fractures and dislocations, and provide long-term stability. Historically, the surgical management of thoracolumbar fractures involved posterior instrumentation and fusion. Recognizing the importance of reducing retropulsed bone fragments in burst fractures led to the use of anterior decompression and fusion, which was eventually combined with anterior internal fixation. The transition from hook-rod constructs to pedicle screw fixation reduced the number of levels involved in instrumentation and arthrodesis. In addition, the use of a combined approach has also been described.
This systematic review attempts to determine if the choice of surgical approach (ie, anterior, posterior, or combined) improves clinical outcomes in patients with thoracic and lumbar fractures. The guideline applies to adults presenting with thoracolumbar fractures requiring surgery and includes patients with or without neurologic deficits. The outcomes of interest include clinical results, neurologic recovery in patients with deficits, radiologic parameters, and complications.
Methods
The Guidelines Task Force initiated a systematic review of the literature relevant to the diagnosis and treatment of patients with thoracolumbar trauma. Through objective evaluation of the evidence and transparency in the process of making recommendations, this evidence-based clinical practice guideline was developed for the diagnosis and treatment of adult patients with thoracolumbar injury. These guidelines are developed for educational purposes to assist practitioners in their clinical decision-making processes. Additional information about the methods used in this systematic review can be found in the introduction and methodology chapter.
Literature Search
The task force members identified search terms and parameters, and a medical librarian implemented the literature search consistent with the literature search protocol (see Appendix I), using the National Library of Medicine PubMed database and the Cochrane Library (which included the Cochrane Database of Systematic Reviews, the Database of Abstracts of Reviews of Effect, the Cochrane Central Register of Controlled Trials, the Health Technology Assessment Database, and the National Health Service Economic Evaluation Database) for the period from January 1, 1946 to March 31, 2015, using the search strategies provided in Appendix I.
The outcomes of interest included clinical outcomes, radiologic results (local kyphosis), and complications. Clinical outcomes, such as pain, neurologic recovery, spine function, and health-related quality of life, were included. Not all the above outcomes were independently analyzed in all of the studies. The radiologic outcome was the Cobb angle across the injured segment at final follow-up. Complications were reported as incidence per group; however, no study reported the severity of complications. Results were reported in this guideline only when statistical analysis was performed.
RESULTS
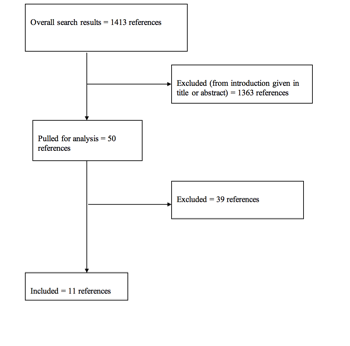
Task Force members reviewed 1413 abstracts yielded from the literature search, and 2 reviewers identified 50 studies for full-text review and extraction, addressing the clinical questions, in accordance with the literature search protocol (Appendix I). Task Force members identified 11 studies to answer the targeted clinical questions. When level I, II, or III literature was available to answer specific questions, the task force did not review level IV studies.
Inclusion/Exclusion Criteria
Articles were retrieved and included only if they met specific inclusion/exclusion criteria. These criteria were also applied to articles provided by Guideline Task Force members who supplemented the electronic database searches with articles from their own files. To reduce bias, these criteria were specified before conducting the literature searches.
Articles that do not meet the following criteria were, for the purposes of this evidence-based clinical practice guideline, excluded. To be included as evidence in the guideline, an article had to be a report of a study that:
- Investigated patients with thoracolumbar injuries;
- Included patients ≥18 years of age;
- Enrolled ≥80% of thoracolumbar injuries (studies with mixed patient populations were included if they reported results separately for each group/patient population);
- Was a full article report of a clinical study;
- Was not an internal medical records review, meeting abstract, historical article, editorial, letter, or commentary;
- Appeared in a peer-reviewed publication or a registry report;
- Enrolled ≥10 patients per arm per intervention (20 total) for each outcome;
- Included only human subjects;
- Was published in or after 1946 through March 31, 2015;
- Quantitatively presented results;
- Was not an in vitro study;
- Was not a biomechanical study;
- Was not performed on cadavers;
- Was published in English;
- Was not a systematic review, meta-analysis, or guideline developed by others*;
- Was a case series (therapeutic study) where higher level evidence exists.
Rating Quality of Evidence
The guideline task force used a modified version of the North American Spine Society’s evidence-based guideline development methodology. The North American Spine Society methodology uses standardized levels of evidence (Appendix III) and grades of recommendation (Appendix IV) to assist practitioners in easily understanding the strength of the evidence and recommendations within the guidelines. The levels of evidence range from level I (high quality randomized controlled trial) to level IV (case series). Grades of recommendation indicate the strength of the recommendations made in the guideline based on the quality of the literature. Levels of evidence have specific criteria and are assigned to studies before developing recommendations. Recommendations are then graded based upon the level of evidence. To better understand how levels of evidence inform the grades of recommendation and the standard nomenclature used within the recommendations, see Appendix IV.
Guideline recommendations were written using a standard language that indicates the strength of the recommendation. “A” recommendations indicate a test or intervention is 2 “recommended”; “B” recommendations “suggest” a test or intervention; “C” recommendations indicate a test or intervention or “is an option.” “Insufficient evidence” statements clearly indicate that “there is insufficient evidence to make a recommendation for or against” a test or intervention. Task force consensus statements clearly state that “in the absence of reliable evidence, it is the task force’s opinion that” a test or intervention may be considered. Both the levels of evidence assigned to each study and the grades of each recommendation were arrived at by consensus of the workgroup employing up to three rounds of voting when necessary.
In evaluating studies as to levels of evidence for this guideline, the study design was interpreted as establishing only a potential level of evidence. As an example, a therapeutic study designed as a randomized controlled trial would be considered a potential level I study. The study would then be further analyzed as to how well the study design was implemented and significant shortcomings in the execution of the study would be used to downgrade the levels of evidence for the study’s conclusions (see Appendix V for additional information and criteria).
Revision Plans
In accordance with the Institute of Medicine’s standards for developing clinical practice guidelines and criteria specified by the National Guideline Clearinghouse, the task force will monitor related publications after the release of this document and will revise the entire document and/or specific sections “if new evidence shows that a recommended intervention causes previously unknown substantial harm; that a new intervention is significantly superior to a previously recommended intervention from an efficacy or harms perspective; or that a recommendation can be applied to new populations.”1 In addition, the task force will confirm within 5 years from the date of publication that the content reflects current clinical practice and the available technologies for the evaluation and treatment for patients with thoracolumbar trauma.
DISCUSSION
Eleven studies were identified as either cohort or randomized clinical trials that compared anterior, posterior, or combined anterior-posterior approaches (see Appendix VI). There were 4 randomized controlled trials that were rated as level II.2-5 All 6 retrospective cohort studies were rated as level III.6-10 One prospective cohort study was rated a level III.11
Ten studies included only thoracolumbar burst fractures and 1 only included fracture dislocations.2 Neurologic injuries varied among the studies with 8 studies including patients with deficits and 3 studies including patients without neurologic deficits.
The anterior approach included corpectomy or partial corpectomy, and reconstruction with strut grafting or cage and anterior instrumentation. If additional posterior instrumentation was used, then the patient was considered to be a combined anterior-posterior approach. The posterior group used pedicle screws except in 2 studies where posterior rod-hook instrumentation was performed. Posterior decompression may have been performed as needed in this group. In addition, 2 studies that used transforaminal interbody decompression and fusion (TLIF) combined with posterior pedicle screw instrumentation were included in the posterior approach group.2,11 The authors could not stratify the results in patients having posterior decompression and instrumentation to posterior instrumentation only. Combined anterior-posterior approach included corpectomy or partial corpectomy, and reconstruction with strut grafting or cage and anterior instrumentation and additional posterior pedicle screw instrumentation.
Seven studies compared anterior to posterior approach: 2 studies were level II, and 5 were level III (see Appendix VI). Five studies compared posterior to combined anterior-posterior approaches, 3 of which were level II and 2 were level III. One study had 3 treatment arms and was included in both the comparisons between anterior and posterior and between posterior and combined approaches.7 There was no literature available to compare anterior only to combined anterior-posterior approach.
Comparison of Anterior versus Posterior Approaches
Clinical Outcomes
There were 7 studies that compared clinical and neurologic outcomes of anterior decompression and fusion to posterior surgery with or without decompression (Table 1). No differences in neurologic outcomes or clinical outcomes were noted in any study.
Radiologic Outcomes
Two studies showed better overall fracture Cobb angle correction at final follow-up with anterior surgery, while 5 studies reported no differences in radiologic outcomes between anterior and posterior approaches. The 2 studies that favored anterior surgery were both level III evidence, while 2 level II and 3 level III studies did not show a difference.
Complications
Complications were reported in 5 studies comparing anterior to posterior surgery. One level II study demonstrated fewer complications and favored the anterior approach, and 1 level II study favored the posterior approach. Three level III studies showed no differences between approaches.
|
Table 1. Anterior versus Posterior Approach
|
|
Clinical Outcomes
|
|
Evidence Level
|
Favors Anterior
|
Favors Posterior
|
No difference
|
|
I
|
|
|
|
|
II
|
|
|
Wood et al,3 Lin et al4
|
|
III
|
|
|
Wu et al,9 Sasso et al,12 Hitchon et al,10 Esses et al,6 Danisa et al7
|
|
IV
|
|
|
|
|
Total
|
|
|
7
|
|
|
|
|
|
|
Radiologic Outcomes
|
|
I
|
|
|
|
|
II
|
|
|
Wood et al,3 Lin et al4
|
|
III
|
Sasso et al,12 Hitchon et al10
|
|
Wu et al,9 Esses et al,6 Danisa et al7
|
|
IV
|
|
|
|
|
Total
|
2
|
|
5
|
|
Complications
|
|
I
|
|
|
|
|
II
|
Wood et al3
|
Lin et al4
|
|
|
III
|
|
|
Hitchon et al,10 Esses et al,6 Danisa et al7
|
|
IV
|
|
|
|
|
Total
|
1
|
1
|
3
|
Comparison of Posterior versus Anterior-Posterior Approach
Five studies compared posterior instrumentation with or without decompression to combined anterior-posterior approaches (Table 2). Two studies were level II randomized controlled trials, 2 studies were level III retrospective cohort study, and 1 study was a level III prospective cohort study.
Clinical Outcomes
Four studies (1 level II and 3 level III) reported no difference in clinical outcomes. One level II study reported better clinical outcomes in the posterior approach, although, despite lower pain, the authors recommended against the posterior only approach because of a high incidence of poor radiologic results. 5
Radiologic Outcomes
One level II and 2 level III studies reported no difference in radiologic outcomes between groups, while 1 level II study and 1 level III favored the anterior-posterior approach.
Complications
Complications occurred more frequently after anterior-posterior fusion compared to posterior approach in 2 level II studies, while all 3 level III studies reported no difference between groups.
|
Table 2. Anterior-Posterior versus Posterior Approach
|
|
|
Clinical outcomes
|
|
Evidence Level
|
Favors
Anterior/ Posterior
|
Favors Posterior
|
No difference
|
|
I
|
|
|
|
|
II
|
|
Korovessis et al5
|
Hao et al2
|
|
III
|
|
|
Schmid et al,11 Danisa et al,7 Been et al8
|
|
IV
|
|
|
|
|
Total
|
|
1
|
4
|
|
|
Radiologic outcomes
|
|
I
|
|
|
|
|
II
|
Korovessis et al5
|
|
Hao et al 2
|
|
III
|
Been et al8
|
|
Danisa et al,7 Schmid et al11
|
|
IV
|
|
|
|
|
Total
|
2
|
|
3
|
|
|
Complications
|
|
I
|
|
|
|
|
II
|
|
Korovessis et al,5 Hao et al2
|
|
|
III
|
|
|
Danisa et al,7 Been et al,8 Schmid et al11
|
|
IV
|
|
|
|
|
Total
|
|
2
|
3
|
|
Question
|
|
Does the choice of surgical approach (anterior, posterior, or combined) improve clinical outcomes in patients with thoracic and lumbar burst fractures?
|
|
Recommendation
|
|
In the surgical treatment of patients with thoracolumbar fractures, physicians may use an anterior, posterior, or a combined approach as the selection of approach does not appear to impact clinical or neurological outcomes.
|
|
Strength of Recommendation: Grade B
|
This recommendation is based on the near uniformity of results of the 4 randomized clinical trials. They did not show any differences in clinical results, including pain and neurologic recovery, between anterior and posterior approaches and only 1 level II study shows improved clinical outcomes in the posterior only treatment group compared to the combined group. The authors of this study recommended against the posterior approach despite having better clinical results because of poorer radiologic outcomes.5
| Recommendation |
|
With regard to radiologic outcome in the surgical treatment of patients with thoracolumbar fractures, physicians may use an anterior, posterior, or combined approach because there is conflicting evidence in the comparison among approaches.
|
|
Strength of Recommendation: Grade Insufficient
|
Comparing anterior to posterior approaches, the radiologic outcomes were not different in the 2 level II studies, while the results were conflicting comparing posterior only to combined anterior-posterior approaches.
|
Recommendation
|
|
With regard to complications in the surgical treatment of patients with thoracolumbar fractures, physicians may use an anterior, posterior, or combined approach as there is conflicting evidence in the comparison among approaches.
|
|
Strength of Recommendation: Grade Insufficient
|
When comparing complications associated with anterior and posterior surgery, there was heterogeneity in the results in 2 level II studies, while all level III studies reported no differences. The combined anterior-posterior approach showed a higher complication risk in 2 of the 3 level II studies and no difference in one level II study.
Future Research
Future research is still needed to determine an optimum surgical approach for thoracolumbar fractures. Although there were 5 randomized controlled trials, these trials had significant deficiencies, including lack of power analysis, lack of description of randomization methods, and absent a priori identification of primary outcome variables. When developing the research plan, the use of the CONSORT method and reporting results is recommended. Many of the studies used outdated surgical techniques, so new studies using modern methods are needed. The results should be stratified based on neurologic injury and fracture types. The new methods to classify thoracolumbar fractures need to be incorporated into study design, and the results should be analyzed according to the severity of injury based on these schemes.
Conclusion
Eleven studies compared outcomes between anterior and posterior approaches and anterior-posterior and posterior approaches. There was moderate evidence that no differences in clinical outcomes based on approach occur. In addition, conflicting evidence was present indicating that minimal differences in radiologic or complication risk exist between approaches. Thus, surgeons may choose any of 3 approaches when deciding optimal surgical treatment for thoracolumbar burst fractures.
Potential Conflicts of Interest
The task force members were required to report all possible conflicts of interest (COIs) prior to beginning work on the guideline, using the COI disclosure form of the AANS/CNS Joint Guidelines Review Committee, including potential COIs that are unrelated to the topic of the guideline. The CNS Guidelines Committee and Guideline Task Force Chairs reviewed the disclosures and either approved or disapproved the nomination. The CNS Guidelines Committee and Guideline Task Force Chairs are given latitude to approve nominations of Task Force members with possible conflicts and address this by restricting the writing and reviewing privileges of that person to topics unrelated to the possible COIs. The conflict of interest findings are provided in detail in the companion introduction and methods manuscript.
Disclaimer of Liability
This clinical systematic review and evidence-based guideline was developed by a multidisciplinary physician volunteer task force and serves as an educational tool designed to provide an accurate review of the subject matter covered. These guidelines are disseminated with the understanding that the recommendations by the authors and consultants who have collaborated in their development are not meant to replace the individualized care and treatment advice from a patient's physician(s). If medical advice or assistance is required, the services of a competent physician should be sought. The proposals contained in these guidelines may not be suitable for use in all circumstances. The choice to implement any particular recommendation contained in these guidelines must be made by a managing physician in light of the situation in each particular patient and on the basis of existing resources.
Disclosures
These evidence-based clinical practice guidelines were funded exclusively by the Congress of Neurological Surgeons and the Section on Disorders of the Spine and Peripheral Nerves in collaboration with the Section on Neurotrauma and Critical Care, which received no funding from outside commercial sources to support the development of this document.
Acknowledgments
The guidelines task force would like to acknowledge the CNS Guidelines Committee for their contributions throughout the development of the guideline and the AANS/CNS Joint Guidelines Review Committee for their review, comments, and suggestions throughout peer review, as well as the contributions of Trish Rehring, MPH, CHES, Senior Manager of Clinical Practice Guidelines for the CNS, and Mary Bodach, MLIS, Guidelines Specialist and Medical Librarian for assistance with the literature searches. Throughout the review process the reviewers and authors were blinded from one another. At this time, the guidelines task force would like to acknowledge the following individual peer reviewers for their contributions: Maya Babu, MD, MBA, Greg Hawryluk, MD, PhD, Steven Kalkanis, MD, Yi Lu, MD, PhD, Jeffrey J. Olson, MD, Martina Stippler, MD, Cheerag Upadhyaya, MD, MSc, and Robert Whitmore, MD.
REFERENCES
1. Ransohoff DF, Pignone M, Sox HC. How to decide whether a clinical practice guideline is trustworthy. JAMA 2013;309:139-40.
2. Hao D, Wang W, Duan K, et al. Two-year follow-up evaluation of surgical treatment for thoracolumbar fracture-dislocation. Spine 2014;39:E1284-E1290.
3. Wood K, Buttermann G, Mehbod A, Garvey T, Jhanjee R, Sechriest V. Operative compared with nonoperative treatment of a thoracolumbar burst fracture without neurological deficit. A prospective, randomized study. J Bone Joint Surg Am 2003;85A:773-781.
4. Lin B, Chen ZW, Guo ZM, Liu H, Yi ZK. Anterior approach versus posterior approach with subtotal corpectomy, decompression, and reconstruction of spine in the treatment of thoracolumbar burst fractures: a prospective randomized controlled study [published online ahead of print Jun 1]. J Spinal Disord Tech.
5. Korovessis P, Baikousis A, Zacharatos S, Petsinis G, Koureas G, Iliopoulos P. Combined anterior plus posterior stabilization versus posterior short-segment instrumentation and fusion for mid-lumbar (L2-L4) burst fractures. Spine 2006;31:859-868.
6. Esses SI, Botsford DJ, Kostuik JP. Evaluation of surgical treatment for burst fractures. Spine 1990;15:667-673.
7. Danisa OA, Shaffrey CI, Jane JA, et al. Surgical approaches for the correction of unstable thoracolumbar burst fractures: a retrospective analysis of treatment outcomes. J Neurosurg 1995;83:977-983.
8. Been HD, Bouma GJ. Comparison of two types of surgery for thoraco-lumbar burst fractures: combined anterior and posterior stabilisation vs. posterior instrumentation only. Acta Neurochir 1999;141:349-357.
9. Wu H, Wang CX, Gu CY, et al. Comparison of three different surgical approaches for treatment of thoracolumbar burst fracture. Chin J Traumatol 2013;16:31-35.
10. Hitchon PW, Torner J, Eichholz KM, Beeler SN. Comparison of anterolateral and posterior approaches in the management of thoracolumbar burst fractures. J Neurosurg Spine 2006;5:117-125.
11. Schmid R, Lindtner RA, Lill M, Blauth M, Krappinger D, Kammerlander C. Combined posteroanterior fusion versus transforaminal lumbar interbody fusion (TLIF) in thoracolumbar burst fractures. Injury 2012;43:475-479.
12. Sasso RC, Renkens K, Hanson D, Reilly T, McGuire Jr RA, Best NM. Unstable thoracolumbar burst fractures: anterior-only versus short-segment posterior fixation. J Spinal Disord Tech 2006;19:242-248.
Appendix I. Literature Searches
Search Strategies
PubMed
1.Lumbar vertebrae [MeSH] OR Thoracic vertebrae [MeSH]
2. Spinal Injuries [MeSH] OR Spinal Cord Injuries [MeSH]
3. #1 AND #2
4. Thoracolumbar [TIAB] OR thoraco-lumbar [TIAB] OR thoraco lumbar [TIAB] OR burst [Title]
5.Injur* [TIAB] OR trauma* [TIAB] OR fractur* [TIAB] OR dislocation* [TIAB]
6. #4 AND #5
7. Lumbar vertebrae/injuries [MeSH] OR Thoracic vertebrae/injuries [MeSH]
8. #3 OR #6 OR #7
9.Orthopedic Procedures [MeSH] OR Neurosurgical Procedures [MeSH] OR Decompression, surgical [MeSH] OR Orthopedic Fixation Devices [MeSH] OR surgery [SH] OR instrumentation [SH]
10.surgery[tiab] OR surgical[tiab] OR operati*[tiab] OR repair*[tiab] OR stabiliz*[tiab] OR fixation[tiab] OR reconstruct*[tiab] OR fusion[tiab] OR decompress*[tiab] OR spondylodes*[tiab] OR spondylosyndes*[tiab] OR arthrodes*[tiab] OR laminectomy[tiab] OR discectomy[tiab] OR diskectomy OR “percutaneous vertebral augmentation”[tiab] OR “bone screw”[tiab] OR “bone screws”[tiab] OR “bone plate”[tiab] OR “bone plates” [tiab] OR “pedicle screw”[tiab] OR “pedicle screws”[tiab]
11. #9 OR #10
12.Thoracoscopy [MeSH] OR Retroperitoneal space [MeSH]
13.Anterior OR Circumferential OR lateral OR Posterior OR Posterolateral OR retroperitoneal OR thoracotomy OR thoracoscop* OR transthoracic OR thoracoabdominal [TIAB]
14.#12 OR #13
15.#11 AND #14
16. #8 AND #15
17. animal [MeSH] NOT human [MeSH]) OR cadaver [MeSH] OR cadaver* [Titl] OR comment [PT] OR letter [PT] OR editorial [PT] OR addresses [PT] OR news [PT] OR “newspaper article” [PT] OR case reports [PT]
18.#16 NOT #17
19.osteoporosis [MH] OR osteoporotic fractures [MH] OR osteoporo* [TITLE] OR spinal neoplasms [MH] OR tumor* [TITLE] OR tumour* [TITLE] OR malignan* [TITLE]
20.#18 NOT #19
21.12.#20 AND English [Lang]
Cochrane Library
1.Lumbar vertebrae: MeSH descriptor, explode all trees
2.Thoracic vertebrae: MeSH descriptor, explode all trees
3.#1 OR #2
4.Spinal Injuries: MeSH descriptor
5.Spinal Cord Injuries: MeSH descriptor
6.#4 OR #5
7.#3 AND #6
8.(Thoracolumbar OR thoraco-lumbar OR thoraco lumbar OR burst) NEAR/4 (Injur* OR trauma* OR fractur* OR dislocation*):ti,ab,kw
9.Lumbar vertebrae/injuries: MeSH descriptor, explode all trees
10.Thoracic vertebrae/injuries: MeSH descriptor, explode all trees
11.>#9 OR #10
12.>#7 OR #8 OR #11
13.>mh osteoporosis or mh osteoporotic fractures or mh spinal neoplasms
14.>osteoporo* or tumor* or malignan*:ti
15.>#13 OR #14
16.#12 NOT #15
Appendix II. Article Inclusions and Exclusions
Included and Excluded Articles Flowchart
Appendix III. Rating Evidence Quality
Levels of Evidence for Primary Research Questiona
|
Types of studies
|
|
|
Therapeutic studies – Investigating the results of treatment
|
Prognostic studies – Investigating the effect of a patient characteristic on the outcome of disease
|
Diagnostic studies – Investigating a diagnostic test
|
Economic and decision analyses – Developing an economic or decision model
|
|
Level I
|
- High-quality randomized trial with statistically significant difference or no statistically significant difference but narrow confidenceintervals
- Systematic reviewb of level I RCTs (and study results were homogenousc)
|
- High-quality prospective studyd (all patients were enrolled at the same point in their disease with
≥80% follow-up of enrolled patients)
- Systematic reviewb of level I studies
|
- Testing of previously developed diagnostic criteria on consecutive patients (with universally applied reference “gold” standard)
- Systematic reviewb of level I studies
|
- Sensible costs and alternatives; values obtained from many studies; with multiway sensitivity analyses
- Systematic reviewb of level I studies
|
|
Level II
|
- Lesser quality RCT (e.g., ≤80% follow-up, no blinding, or improper randomization)
- Prospectived comparative studye
- Systematic reviewb of level II studies or level I studies with inconsistent results
|
- Retrospectivef study
- Untreated controls from an RCT
- Lesser quality prospective study (e.g., patients enrolled at different points in their disease or
≤80% follow-up)
- Systematic reviewb of level II studies
|
- Development of diagnostic criteria on consecutive patients (with universally applied reference “gold” standard)
- Systematic reviewb of level II studies
|
- Sensible costs and alternatives; values obtained from limited studies; with multiway sensitivity analyses
- Systematic reviewb of level II studies
|
|
Level III
|
- Case control studyg
- Retrospectivef comparative studye
- Systematic reviewb of level III studies
|
|
- Study of non consecutive patients; without consistently applied reference “gold” standard
- Systematic reviewb of level III studies
|
- Analyses based on limited alternatives and costs; and poor estimates
- Systematic reviewb of level III studies
|
|
Level IV
|
Case seriesh
|
Case series
|
- Case-control study
- Poor reference standard
|
- Analyses with no sensitivity analyses
|
RCT, Randomized controlled trial.
aA complete assessment of quality of individual studies requires critical appraisal of all aspects of the study design.
bA combination of results from ≥2 previous studies.
cStudies provided consistent results.
dStudy was started before the first patient enrolled.
ePatients treated one way (e.g., instrumented arthrodesis) compared with a group of patients treated in another way (e.g., unsintrumented arthrodesis) at the same institution.
fThe study was started after the first patient enrolled.
gPatients identified for the study based on their outcome, called “cases” (e.g., pseudoarthrosis) are compared to those who did not have outcome, called “controls” (e.g., successful fusion).
hPatients treated one way with no comparison group of patients treated in another way.
Appendix IV. Linking Levels of Evidence to Grades of Recommendation
|
Grade of Recommendation
|
Standard Language
|
Levels of Evidence
|
|
A
|
Recommended
|
Two or more consistent level I studies
|
|
B
|
Suggested
|
One level I study with additional supporting level II or III studies
|
Two or more consistent level II or III studies
|
|
C
|
Is an option
|
One level I, II, or III study with supporting level IV studies
|
Two or more consistent level IV studies
|
|
Insufficient
(insufficient or conflicting evidence)
|
Insufficient evidence to make recommendation for or against
|
A single level I, II, III, or IV study without other supporting evidence
|
>1 study with inconsistent findingsa
|
aNote that in the presence of multiple consistent studies, and a single outlying, inconsistent study, the Grade of Recommendation will be based on the level of the consistent studies.
Appendix V. Criteria Grading the Evidence
The task force used the criteria provided below to identify the strengths and weaknesses of the studies included in this guideline. Studies containing deficiencies were downgraded one level (no further downgrading allowed, unless so severe that study had to be excluded). Studies with no deficiencies based on study design and contained clinical information that dramatically altered current medical perceptions of topic were upgraded.
- Baseline study design (i.e., therapeutic, diagnostic, prognostic) determined to assign initial level of evidence.
- Therapeutic studies reviewed for following deficiencies:
- Failure to provide a power calculation for an RCT;
- High degree of variance or heterogeneity in patient populations with respect to presenting diagnosis/demographics or treatments applied;
- <80% of patient follow-up;
- Failure to utilize validated outcomes instrument;
- No statistical analysis of results;
- Cross over rate between treatment groups of >20%;
- Inadequate reporting of baseline demographic data;
- Small patient cohorts (relative to observed effects);
- Failure to describe method of randomization;
- Failure to provide flowchart following patients through course of study (RCT);
- Failure to account for patients lost to follow-up;
- Lack of independent post-treatment assessment (e.g., clinical, fusion status, etc.);
- Utilization of inferior control group:
- Historical controls;
- Simultaneous application of intervention and control within same patient.
- Failure to standardize surgical/intervention technique;
- Inadequate radiographic technique to determine fusion status (e.g., static radiographs for instrumented fusion).
- Methodology of diagnostic studies reviewed for following deficiencies:
- Failure to determine specificity and sensitivity;
- Failure to determine inter- and intraobserver reliability;
- Failure to provide correlation coefficient in the form of kappa values.
- Methodology of prognostic studies reviewed for following deficiencies:
- High degree of variance or heterogeneity in patient populations with respect to presenting diagnosis/demographics or treatments applied;
- Failure to appropriately define and assess independent and dependent variables (e.g., failure to use validated outcome measures when available).
Appendix VI. Evidence Table
|
Author, Year
|
Level of Evidence
|
Task Force Conclusions Relative to Question and Rationale for Evidence Grading
|
|
Been et al.,8 1999
|
III
|
This paper compared anterior-posterior to posterior approaches: the clinical outcome was similar in both groups but greater loss of correction occurred in posterior only group
|
|
Danisa et al.,7 1995
|
III
|
This paper compared anterior-posterior to posterior approaches: no differences in clinical outcomes, complications, and deformity correction
|
|
Esses et al.,6 1990
|
III
|
This paper compared anterior to posterior approaches: no difference in neurologic recovery, complications, or deformity correction
|
|
Hao et al.,2 2014
|
II
|
This paper compared anterior to posterior (TLIF) approaches: no difference in clinical and radiologic outcomes, lower complications in posterior approach
|
|
Hitchon et al.,10 2006
|
III
|
This paper compared anterior to posterior approaches: no difference in clinical outcomes and complications. Angular deformity is more successfully corrected and maintained in anterior technique
|
|
Korovessis et al.,5
2006
|
II
|
This paper compared anterior-posterior to posterior approaches: despite having better clinical outcomes and fewer complications, short segment posterior instrumentation did not adequately stabilize mid-lumbar burst fractures compared to anterior-posterior approach
|
|
Lin et al.,4 2011
|
II
|
This paper compared anterior to posterior approaches: both procedures approaches have similar clinical and radiographic results, although the posterior had fewer complications and better pulmonary function
|
|
Sasso et al.,12 2006
|
III
|
This paper compared anterior to posterior approaches: both procedures approaches have similar clinical results and risk of complications. The anterior group had better radiologic results
|
|
Schmid et al.,11
2012
|
III
|
This paper compared anterior to posterior (TLIF) approaches: no difference in clinical, radiologic outcomes, and complications between groups
|
|
Wood et al.,3 2005
|
II
|
This paper compared anterior to posterior approaches: no differences in clinical and radiologic results between groups. Posterior approach was associated with higher complications
|
|
Wu et al.,9 2013
|
III
|
This paper compared anterior to posterior approaches: no difference in clinical and radiologic results
|
© Congress of Neurological Surgeons
Source: Neurosurgery, September 6, 2018