Sponsored by: Congress of Neurological Surgeons (CNS) and the Section on Pediatric Neurosurgery
Endorsed by: The Congress of Neurological Surgeons (CNS), American Association of Neurological Surgeons (AANS), and Spina Bifida Association (SBA)
Catherine A. Mazzola, MD1, Nadege Assassi2, Lissa C. Baird, MD3, David F. Bauer, MD4, Alexandra D. Beier, DO5, Jeffrey P. Blount, MD6, Susan R. Durham, MD, MS7, Ann Marie Flannery, MD8, Paul Klimo Jr., MD9, Catherine McClung-Smith, MD10, Dimitrios C. Nikas, MD11, Patricia Rehring, MPH12, Mandeep S. Tamber, MD, PhD13, Rachana Tyagi, MD14
- Goryeb Children’s Hospital, Morristown, New Jersey; Rutgers Department of Neurological Surgery, Newark, New Jersey
- Department of Surgery, Division of Neurosurgery, Robert Wood Johnson Medical School, New Brunswick, New Jersey
- Department of Neurological Surgery, Oregon Health and Science University, Portland, Oregon
- Department of Surgery, Division of Neurosurgery, Dartmouth-Hitchcock Medical Center, Lebanon, New Hampshire
- Division of Pediatric Neurosurgery, University of Florida Health Jacksonville, Jacksonville, Florida
- Division of Pediatric Neurosurgery, Department of Neurosurgery, University of Alabama at Birmingham; Children’s of Alabama, Birmingham, Alabama
- University of Vermont, Division of Neurosurgery, Burlington, Vermont
- Kids Specialty Center, Women’s & Children’s Hospital, Lafayette, Louisiana
- Semmes-Murphey; Department of Neurosurgery, University of Tennessee Health Science Center; Le Bonheur Children’s Hospital, Memphis, Tennessee
- Department of Neurological Surgery, Palmetto Health USC Medical Group, Columbia, South Carolina
- Division of Pediatric Neurosurgery, Advocate Children's Hospital, Oak Lawn, Illinois
- Congress of Neurological Surgeons, Schaumburg, Illinois
- Division of Pediatric Neurosurgery, British Columbia Children’s Hospital, University of British Columbia, Vancouver, British Columbia, Canada
- Department of Neurosurgery, Mercer University Medical School, Macon, Georgia
Correspondence:
Catherine A. Mazzola, MD
Rutgers New Jersey Medical School
Newark, New Jersey
E-mail: catherine.mazzola@rutgers.edu
Abbreviations:
AANS - American Association of Neurological Surgeons (AANS)
CNS - Congress of Neurological Surgeons
CPC - choroid plexus coagulation
ETV - endoscopic third ventriculostomies
ICBDSR - International Clearinghouse for Birth Defects Surveillance and Research
ICD - International Classification of Disease
IOM - Institute of Medicine
MOMS - Management of Myelomeningocele Study
MM - myelomeningocele
NIH - National Institute of Health
PRISMA - Preferred Reporting Items for Systematic Reviews and Meta-Analyses
SB – spina bifida
VPS - ventriculoperitoneal shunt
WHO- World Health Organization
ABSTRACT
Background: There are 1,500 to 2,000 infants born annually in the United States with spina bifida (SB). The incidence of SB in the developing world is much higher because of malnutrition and folic acid deficiency during pregnancy. Recent advances in medicine and technology have made prenatal repair of myelomeningocele (MM) possible.
Objective: The objectives of the guidelines are to (1) create clinical recommendations for best practices, based on a systematic review and analysis of available literature relevant to MM closure, (2) to obtain a multi-disciplinary endorsement of these guidelines from relevant organizations, and to (3) disseminate the educational content to physicians of all disciplines to improve the care of infants with MM.
Methods: The Guidelines Task Force developed search terms and strategies used to search PubMed and Embase for relevant literature published between 1966 to September 2016. Strict inclusion/exclusion criteria were used to screen abstracts and to develop a list of relevant articles for full-text review. Full text articles were then reviewed and when appropriate, included as evidence.
Results: Guidelines authors aimed to systematically review the literature and make evidence based recommendations about the timing of closure after birth, hydrocephalus, the impact of prenatal closure, and the effect of prenatal closure on ambulation ability and tethered spinal cord. Evidence concerning persistent ventriculomegaly and cognitive impairment was also evaluated. Hundreds of abstracts were identified and reviewed for each of the five topics. Full text articles were selected for further analysis. A total of 14 studies met stringent inclusion criteria.
Conclusions: The authors created clinical practice guidelines for pediatric myelomeningocele. Based on a comprehensive systematic review, a total of 5 recommendations we developed, including 1 Level I, 2 Level II and 2 Level III recommendations. The guidelines also highlight areas where there is currently insufficient evidence to develop recommendations and more research is needed.
Keywords: Fetal, guidelines, in utero, myelomeningocele, postnatal, spina bifida, tethered cord syndrome
RECOMMENDATIONS
PICO Question: Is there a difference in the proportion of patients who develop shunt-dependent hydrocephalus between fetuses who underwent prenatal myelomeningocele closure compared to infants who underwent postnatal myelomeningocele repair?
Target Population: Infants with myelomeningocele who meet eligibility criteria as fetuses for prenatal myelomeningocele repair.
Recommendation(s): Prenatal repair of myelomeningocele is recommended for those fetuses who meet maternal and fetal MOMS specified criteria for prenatal surgery to reduce the risk of developing shunt-dependent hydrocephalus (Level I). Differences between prenatal and postnatal repair with respect to the requirement for permanent cerebrospinal fluid diversion should be considered along with other relevant maternal and fetal factors when deciding upon a preferred method of myelomeningocele closure.
PICO Question: In patients with myelomeningocele, does prenatal or postnatal closure improve the ability to ambulate?
Target Population: Myelomeningocele patients diagnosed prenatally.
Recommendation(s)
- When possible, for prenatally diagnosed fetuses with myelomeningocele who meet maternal and fetal MOMS study inclusion criteria, prenatal closure of myelomeningocele should be performed, which may improve ambulatory status for patients in the short term (at 30 months of age) (Level II).
- Long term benefit for ambulatory status with prenatal closure is unknown. Children who have had either prenatal or postnatal closure should be carefully followed for the development of tethered spinal cord with the associated loss of ambulatory function (Level III).
PICO Question: In patients born with a myelomeningocele, does closure of the defect within 48 hours reduce the rate of infection?
Target Population: Infants born with a myelomeningocele.
Recommendation(s):
- There is insufficient evidence to confirm that closure of myelomeningoceles within 48 hours decreases the risk of wound infection.
- It is recommended that if myelomeningocele closure is delayed beyond 48 hours, antibiotics should be initiated. (Level III)
PICO Question: In myelomeningocele patients with hydrocephalus, does persistent enlargement of the ventricles adversely impact neurocognitive development?
Target Population: Myelomeningocele patients with hydrocephalus.
Recommendation: Currently, there is insufficient data to conclude that ventricular size and morphology impact neurocognitive development.
PICO Question: Is there a difference in the rate of development of tethered cord syndrome in infants who had prenatal myelomeningocele closure compared to infants who had myelomeningocele closure after birth?
Target Population: Infants and children with myelomeningocele.
Recommendation(s): Continued surveillance for tethered cord syndrome and/or the development of inclusion cysts in children with prenatal and postnatal closure of myelomeningocele is indicated (Level II), as there is evidence that prenatal closure increases the risk of recurrent tethered cord over the baseline rate seen with postnatal closure.
INTRODUCTION
According to the National Institute of Health (NIH), spina bifida (SB) is the “most common type of neural tube defect” and “myelomeningocele (MM) is the most severe and also the most common form of SB”.1 Approximately 1,500 babies are born in the in the United States every year with SB.2 The NIH also estimates approximately 166,000 individuals currently live with SB, in the United States.3 Data from the National Birth Defects Prevention Network also shows a higher reported incidence in Hispanic women (3.80 per 10,000 live births) than in Non-Hispanic black or African-American women (2.73 per 10,000 live births) or in women identified as Non-Hispanic white (3.09 per 10,000 live births).2 It is also important to note the incidence of SB in the world is likely under-reported, due to the limitations of surveillance data collection. Recent changes in the International Classification of Disease (ICD) coding system from ICD9 to ICD10 may also contribute to the under-reporting of SB internationally.4 The risk of disease is also higher in vulnerable populations (women with low socioeconomic status and/or women who reside in low socioeconomic status areas) where mothers of infants with SB often do not receive the necessary health care or access to adequate vitamins and nutrition.5 Research has shown SB patient outcomes are poorer in patients without private insurance.6 SB drastically affects development and quality of life. Infants who are born with MM have a death rate of approximately 10% in infancy, according to the Management of Myelomeningocele Study (MOMS).7
Throughout the world, birth defects data collection is conducted by the International Clearinghouse for Birth Defects Surveillance and Research (ICBDSR), a voluntary non-profit organization affiliated with the World Health Organization (WHO).8 The WHO, which was established in 1974, has identified 45 birth defects surveillance programs globally that are members of ICBDSR. Low to moderate income countries have a higher prevalence of infants and children with SB/MM and other disabilities than higher-income countries. Research has shown mandatory folic acid fortification reduces the incidence of SB in studied populations.2 Atta et al published an article in 2016 clearly showing that legislation enforcing folic acid fortification reduces the incidence of SB, demonstrating SB is significantly more common in world regions without government mandated folic acid fortification of the food supply (ie, Africa, Asia, and Europe).2, 9
The burden of disease is substantial. SB affects development and quality of life. Children with MM require surgical intervention at birth to close the spinal defect, yet many infants born in third world countries lack access to appropriate medical care. Most infants with MM have hydrocephalus and require surgical treatment.
There is currently little agreement among leading practitioners about the optimal timing of closure of the MM defect of the spine. There are differences in practice with regards to team approach to closure, type of closure techniques, administration of antibiotics, and benefits of amputation or preservation of the neural placode. Additionally, as technology advances, in utero (or fetal) closure of the MM defect has been advocated by many experts, but the long-term positive and negative effects of in utero closure have not been well studied. While in utero closure of MM is an option for some pregnant women whose infants met criteria for diagnosis of SB as fetuses, globally, this option is not readily available. Additionally, the effects of hydrocephalus and ventriculomegaly on infants and children with SB have not been well reported. Some experts advocate choroid plexus coagulation and endoscopic third ventriculostomies (ETV). Others have expressed concerns about the long-term efficacy of these options and opt instead to insert a ventriculoperitoneal shunt (VPS) at birth. Other experts advocate conservative non-surgical management of hydrocephalus and ventriculomegaly because of possible complications of VPS.10-12
This systematic review was conducted to evaluate all available evidence to aid clinicians and guide clinical practice by determining the best options for management of pediatric MM. In undertaking this review, the task force defines the condition SB as those infants born with MM. Closed dysraphic conditions such as lipoma, dermal sinus tracts and the split cord anomalies (SCM1, SCM2) are not considered here. For purposes of the literature search, the task force defined “pediatric” as infants, children, and adolescents less than 18 years of age.
This effort was initiated by the Section of Pediatric Neurological Surgeons of the American Association of Neurological Surgeons (AANS) and the Congress of Neurological Surgeons (CNS). The Guidelines Task Force also recruited from a variety of institutions and subspecialty disciplines in an effort to have as broad a representation of opinions and expertise as possible, with the goal of following the IOM recommendations to be inclusive and inter-disciplinary when constructing our guidelines and subsequent recommendations.13 The creation of this document was guided by the understanding that to be effective and trustworthy, guidelines, as created by this Guidelines Task Force, must adhere to best practices. Additionally, the Guidelines Task Force followed protocols established by the Joint Guidelines Review Committee of the AANS and CNS. A conscientious effort was made to be sure that any conflict of interest was avoided. Members who had published extensively in certain areas were mindfully assigned to evaluate evidence in other topics. Every effort was made to ensure that the work product would be accurate, reliable and non-biased.
OBJECTIVES
Guidelines authors aimed to systematically review the literature and make evidence based recommendations about the timing of closure after birth, and to investigate the evidence concerning persistent ventriculomegaly and cognitive impairment.
METHODOLOGY
Process Overview
The Guideline Task Force members conducted a systematic review of the literature relevant to the management of MM in infants and children. Additional details of the systematic review are provided below.
Selection of Clinical Topics
The goals of this effort were to discern the most effective strategies for a variety of MM-related problems, including the timing and type of closure for MM. The authors also considered the use of technical advances such as in utero or fetal closure, closure techniques, endoscopic treatment of hydrocephalus/ventriculomegaly, and other factors affecting infants and children with MM. It is the Guideline Task Force’s aim that these systematic reviews and subsequent evidence based recommendations will lead to improvement in the quality of life for infants and children with MM.
Literature Search
The Guidelines Task Force worked with a research librarian to assist with the formulation of search terms and strategies used to search The National Library of Medicine PubMed and Embase databases for relevant literature published between 1966 to September 2016. Authors also used the article inclusion/exclusion criteria described below to screen abstracts and provide a list of relevant articles for full-text review. Staff compiled the lists for review and final approval by all the Guidelines Task Force members.
Literature searches of electronic databases were supplemented with manual screenings of the bibliographies of all retrieved publications and other potentially relevant systematic reviews where indicated. All literature identified either by searches of the electronic databases or manual searches were subject to the article inclusion/exclusion criteria listed below. The search strategies used are provided within the methods sections of the topics evaluated below.
Article Inclusion/Exclusion Criteria
Articles were retrieved and included as evidence to support the topics discussed in this review if they met specific inclusion/exclusion criteria. These criteria were also applied to articles provided by the Guidelines Task Force who supplemented the electronic database searches with articles from manual searches of the bibliographies of articles. To reduce bias, these criteria were specified before conducting the literature searches. For the purposes of this evidence review, articles that did not meet the following criteria are not evidence and not considered as potential evidence to support the topics and clinical recommendations.
To be included in our review, an article had to meet the following criteria:
- At least 80% of patients had to be patients with MM and <18 years of age.
- Studies that enrolled >20% of patients with other forms of SB were excluded.
- Studies that combined the results of patients with other forms of SB were excluded if the study enrolled less than 80% of target patient population.
- Studies that enrolled mixed patient populations were included only if they reported separate results for the target population. The results of the target population were the only results considered as evidence to support our recommendations.
- The study was a full article report of a clinical study.
- The study was not a meeting abstract, editorial, letter, or a commentary.
- Prospective case series had to report baseline values, if applicable.
- Case series studies with non-consecutive enrollment of patients were excluded.
- Studies had to have appeared in a peer-reviewed publication or a registry report.
- Studies had to enroll at least 10 patients for each distinct outcome measured. If it was a comparative study, a minimum enrollment of 5 patients per treatment arm for each outcome was necessary.
- The study involved humans.
- The study was published between January 1966 and September 2016.
- The study presented results quantitatively.
- The study did not involve "in vitro", "biomechanical" or results performed on cadavers.
- The study was published in English.
- Papers reporting results of systematic reviews, meta-analyses, or guidelines developed by others were excluded.
- Authors specifically excluded follow-up studies in which a cohort of patients from an initial study were followed in time and separately reported upon in a subsequent publication. This prevented the same patients from being included multiple times in this review.
Systematic reviews or meta-analyses conducted by others, or guidelines developed by others were not included as evidence to support this review due to the differences in article inclusion/exclusion criteria specified compared to the criteria specified by the Guidelines Task Force. Although these articles were not included as evidence to support the review, these articles were recalled for full-text review in order for the Guidelines Task Force to conduct manual searches of the bibliographies.
Statistical Methods
In some sections, there was a sufficient quality and quantity of literature to allow more detailed statistical analysis going beyond the basic methods described above. Those topic chapters describe their methods separately.
Rating the Quality of Evidence
The quality of evidence was rated using an evidence hierarchy developed by the Joint AANS/CNS Guidelines Review Committee for 3 different study types including therapeutic effectiveness and diagnosis and prognosis (Appendix II). Additional information regarding the hierarchy classification of evidence can be located here on the CNS Guidelines methodology page.
Strength of Recommendations Rating Scheme
The task force used the methodologies endorsed by the AANS/CNS Guidelines Committee to assign strength to each recommendation in this review. Linking evidence to recommendations, through the utilization of evidentiary tables, has been endorsed by the American Medical Association (AMA), the American Association of Neurological Surgeons (AANS), and the Congress of Neurological Surgeons (CNS). This process validates and supports the relationship between the strength of evidence and the strength of recommendations. Demonstrating the highest degree of clinical certainty, Class I evidence is used to support recommendations of the strongest type, defined as Level I recommendations. Level II recommendations reflect a moderate degree of clinical certainty and are supported by Class II evidence or strong consensus of Class III evidence. Level III recommendations denote clinical uncertainty supported by inconclusive or conflicting evidence or expert opinion. (See Appendix II).
Future Research
The Guidelines Task Force acknowledges that this effort is preliminary and an initial effort designed to begin to explore the literature and the topic. During the course of creation of this document, it was abundantly clear that additional research would soon impact some of the recommendations. Some of the recommendations could also be better defined contracted or expanded to better reflect the necessary information for the treatment of pediatric SB. In accordance with the IOM’s standards for developing clinical practice guidelines, the Guidelines Task Force will monitor related publications following the release of this document and will revise specific sections or the entire document “if new evidence shows that a recommended intervention causes previously unknown substantial harm; that a new intervention is significantly superior to a previously recommended intervention from an efficacy or harms perspective; or that a recommendation can be applied to new populations.”14 In addition, the Guidelines Task Force will confirm within 5 years from the date of publication that the content is current in accordance to current clinical practice and available technologies for the treatment of MM.
CONCLUSION
This evidence based guideline and systematic review of the literature relevant to infants and children with MM were accomplished in order to hopefully improve the quality of life for patients with MM globally. The life-long effects of MM are profound and complex, and for children living in third world nations, may prove fatal, in many cases. It is through continued critical research efforts as specialists who treat these children that possibly one day researchers may find better treatment and eventually, a cure for MM.
Conflicts of Interest
All Guideline Task Force members were required to disclose all potential COIs prior to beginning work on the guideline, using the COI disclosure form of the AANS/CNS Joint Guidelines Review Committee. The CNS Guidelines Committee and Guideline Task Force Chair reviewed the disclosures and either approved or disapproved the nomination and participation on the task force. The CNS Guidelines Committee and Guideline Task Force Chair may approve nominations of task force members with possible conflicts and restrict the writing, reviewing, and/or voting privileges of that person to topics that are unrelated to the possible COIs. See Appendix I for a complete list of disclosures.
Disclosures
These evidence-based clinical practice guidelines were funded exclusively by the Congress of Neurological Surgeons, which received no funding from outside commercial sources to support the development of this document.
Disclaimer of Liability
This clinical, systematic, evidence-based clinical practice guideline was developed by a multi-disciplinary physician volunteer taskforce and is provided as an educational tool based on an assessment of the current scientific and clinical information regarding the management and treatment of pediatric patients with MM. These guidelines are disseminated with the understanding that the recommendations by the authors and consultants who have collaborated in their development are not meant to replace the individualized care and treatment advice from a patient's physician(s). If medical advice or assistance is required, the services of a physician should be sought. The proposals contained in these guidelines may not be suitable for use in all circumstances. The choice to implement any particular recommendation contained in these guidelines must be made by a managing physician in light of the situation in each particular patient and on the basis of existing resources.
ACKNOWLEDGMENTS
The guidelines task force would like to acknowledge the Congress of Neurological Surgeons Guidelines Committee for their contributions throughout the development of the guideline, the American Association of Neurological Surgeons/Congress of Neurological Surgeons Joint Guidelines Review Committee, as well as the American Academy of Pediatrics, Child Neurology Society and Spina Bifida Association for their review, comments, and suggestions throughout peer review, as well as the contributions of Trish Rehring, MPH, CHES, Senior Manager of Clinical Practice Guidelines for the CNS, and Gretchen Kuntz, MSW, MLIS, for assistance with the literature searches. Throughout the review process, the reviewers and authors were blinded from one another. At this time the guidelines task force would like to acknowledge the following individual peer reviewers for their contributions: Kimon Bekelis, MD; Robin Bowman, MD; Timothy J. Brei, MD; Andrew P. Carlson, MD; John Chi, MD; Mark Dias, MD; Jeffrey Olson, MD; John O’Toole, MD; Michael Partington, MD; Curtis Rozzelle, MD; Krystal Tomei, MD; Jan B. Wollack, MD, PhD.
Appendix I. Conflict of Interest Disclosures
The authors have no disclosures.
Appendix II. Rating Evidence Quality
Classification of Evidence on Diagnosis
| Class I Evidence Level I (or A) Recommendation |
Evidence provided by one or more well-designed clinical studies of a diverse population using a “gold standard” reference test in a blinded evaluation appropriate for the diagnostic applications and enabling the assessment of sensitivity, specificity, positive and negative predictive values, and, where applicable, likelihood ratios. |
| Class II Evidence Level II (or B) Recommendation |
Evidence provided by one or more well-designed clinical studies of a restricted population using a “gold standard” reference test in a blinded evaluation appropriate for the diagnostic applications and enabling the assessment of sensitivity, specificity, positive and negative predictive values, and, where applicable, likelihood ratios. |
| Class III Evidence Level III (or C) Recommendation |
Evidence provided by expert opinion or studies that do not meet the criteria for the delineation of sensitivity, specificity, positive and negative predictive values, and, where applicable, likelihood ratios. |
Classification of Evidence on Therapeutic Effectiveness
| Class I Evidence Level I (or A) Recommendation |
Evidence from one or more-well designed, randomized controlled clinical trial, including overviews of such trials. |
| Class II EvidenceLevel II (or B) Recommendation |
Evidence from one or more well-designed comparative clinical studies, such as non-randomized cohort studies, case-control studies, and other comparable studies, including less well-designed randomized controlled trials. |
| Class III Evidence Level III (or C) Recommendation |
Evidence from case series, comparative studies with historical controls, case reports, and expert opinion, as well as significantly flawed randomized controlled trials. |
Classification of Evidence on Prognosis
| Class I Evidence Level I Recommendation |
All 5 technical criteria above are satisfied. |
| Class II Evidence Level II Recommendation |
Four of five technical criteria are satisfied. |
| Class III Evidence Level III Recommendation |
Everything else. |
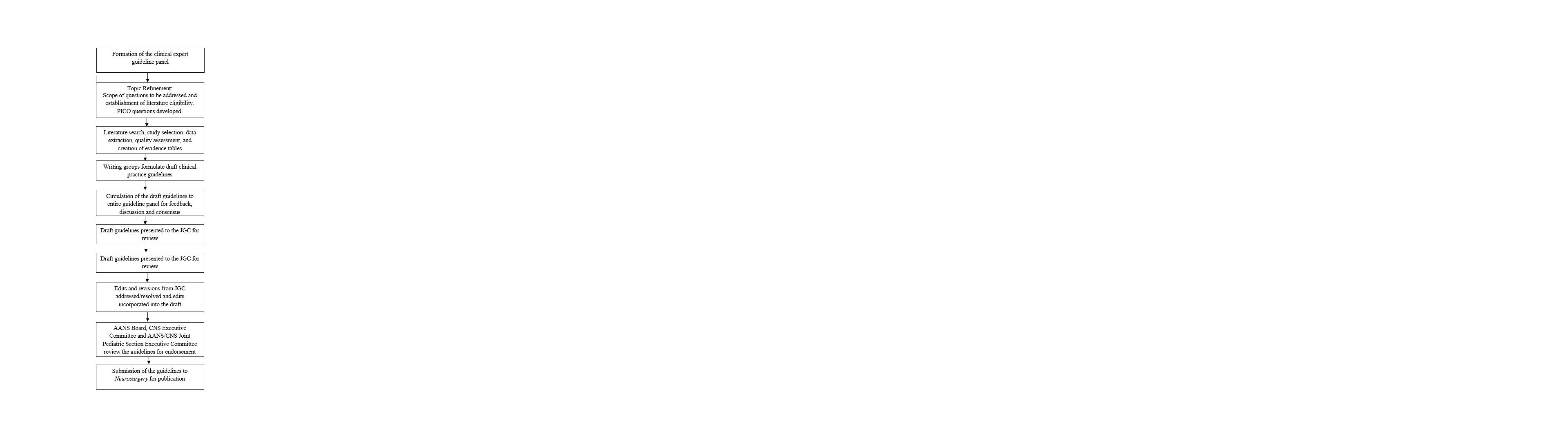
Appendix III: Evidence based guideline development process
REFERENCES
- Eunice Kennedy Shriver National Institute of Child Health and Human Development. About Neural Tube Defects (NTDs). 2018; https://www.nichd.nih.gov/health/topics/ntds/conditioninfo. Accessed December 31, 2018.
- Centers for Disease Control and Prevention. Data & Statistics on Spina Bifida. 2018; https://www.cdc.gov/ncbddd/spinabifida/data.html. Accessed December 31, 2018.
- National Institute of Neurological Disorders and Stroke. Spina Bifida Fact Sheet. 2018; https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Spina-Bifida-Fact-Sheet. Accessed December 31, 2018.
- ICD10Data.com. Spina bifida. 2018; https://www.icd10data.com/ICD10CM/Codes/Q00-Q99/Q00-Q07/Q05-. Accessed December 31, 2018.
- Wasserman CR, Shaw GM, Selvin S, Gould JB, Syme SL. Socioeconomic status, neighborhood social conditions, and neural tube defects. Am. J. Public Health. Nov 1998;88(11):1674-1680.
- Schechter MS, Liu T, Soe M, Swanson M, Ward E, Thibadeau J. Sociodemographic attributes and spina bifida outcomes. Pediatrics. Apr 2015;135(4):e957-964.
- Adzick NS, Thom EA, Spong CY, et al. A randomized trial of prenatal versus postnatal repair of myelomeningocele. N. Engl. J. Med. Mar 17 2011;364(11):993-1004.
- Mburia-Mwalili A, Yang W. Birth Defects Surveillance in the United States: Challenges and Implications of International Classification of Diseases, Tenth Revision, Clinical Modification Implementation. Int Sch Res Notices. 2014;2014:212874.
- Atta CA, Fiest KM, Frolkis AD, et al. Global Birth Prevalence of Spina Bifida by Folic Acid Fortification Status: A Systematic Review and Meta-Analysis. Am. J. Public Health. Jan 2016;106(1):e24-34.
- Shurtleff DB, Luthy DA, Nyberg DA, Benedetti TJ, Mack LA. Meningomyelocele: management in utero and post natum. Ciba Found. Symp. 1994;181:270-280; discussion 280-276.
- Hunt GM. 'The median survival time in open spina bifida'. Dev. Med. Child Neurol. Aug 1997;39(8):568.
- Manning SM, Jennings R, Madsen JR. Pathophysiology, prevention, and potential treatment of neural tube defects. Ment Retard Dev Disabil Res Rev. 2000;6(1):6-14.
- Institute of Medicine Committee on Standards for Developing Trustworthy Clinical Practice G. In: Graham R, Mancher M, Miller Wolman D, Greenfield S, Steinberg E, eds. Clinical Practice Guidelines We Can Trust. Washington (DC): National Academies Press (US); 2011.
- Ransohoff DF, Pignone M, Sox HC. How to decide whether a clinical practice guideline is trustworthy. JAMA. Jan 9 2013;309(2):139-140.